Medicine, Dentistry, and Pharmacy
May 31, 2022
Vitamin D may restore the body's natural barrier against ovarian cancer
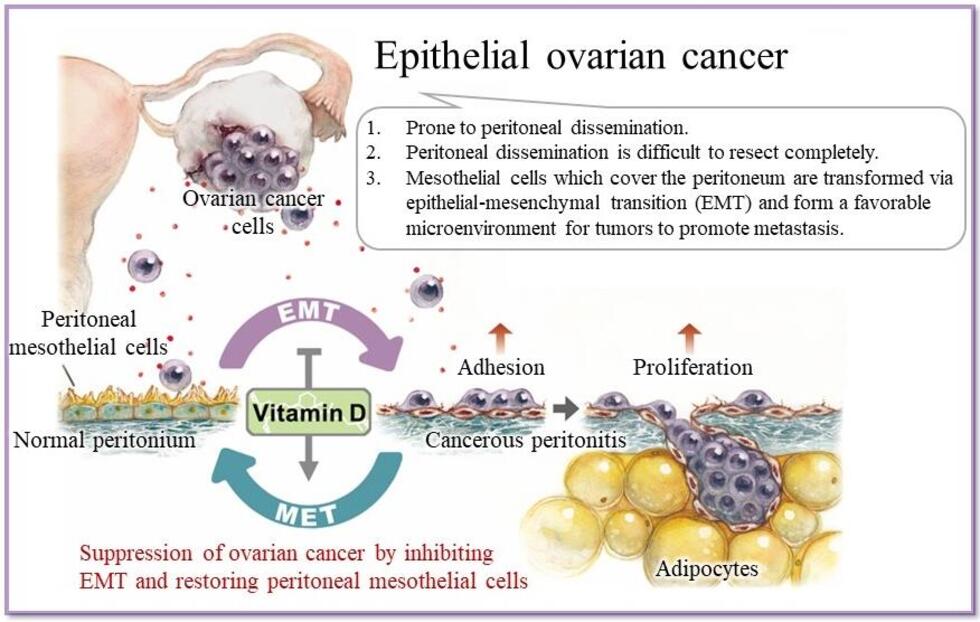
Ovarian cancer has one of the highest death rates of all cancers. One reason for this is that the cancer turns the body’s defenses against itself. However, new research from Nagoya University published in Matrix Biology suggests that vitamin D can effectively prevent one of the key pathways used by this cancer.
Ovarian cancer often undergoes a process called peritoneal metastasis. In this process, its cells detach from their primary site in the ovary and travel to a secondary implantation site, such as the peritoneal wall or diaphragm. The peritoneum defends against this process using a barrier consisting of mesothelial cells, which prevent the adhesion of cancer cells and limit their spread. However, ovarian cancer gets around this defense by transforming the protective mesothelial cells into cancer-associated mesothelial cells. This creates an environment that helps metastasis, assisting the spread of cancer around the body.
The group, led by Dr. Masato Yoshihara of the Department of Obstetrics and Gynecology in collaboration with colleagues at the Bell Research Center and the Department of Pathology at Nagoya University Graduate School of Medicine, found that vitamin D not only counteracted this process but also restored cancer-associated mesothelial cells to their original state. This process strengthened the barrier effect of mesothelial cells and reduced further spread of the cancer. Their study suggests that vitamin D therapy may be a useful addition to the treatment of ovarian cancer.
“We showed the potential of vitamin D for normalizing cancer-associated mesothelial cells, which is the first study of this kind,” said Dr. Kazuhisa Kitami, the first author of the study. “This study's most interesting point is that in situations where early detection of ovarian cancer is still extremely difficult, we showed that the peritoneal environment can be restored to its normal state where it prevents the adhesion and growth of cancer cells.”
Vitamin D can do this because of the complicated way cancer spreads. Previous studies found that cancer cells secrete a protein called TGF-β1, which is associated with cell growth. This also increases the amount of another protein, thrombospondin-1, through the TGF-β/Smad pathway. Thrombospondin-1 has long interested researchers of ovarian cancer because it is found in higher amounts in the later, more deadly stages of cancer. In ovarian cancer, thrombospondin-1 is a key protein that enhances the adhesion and proliferation of ovarian cancer cells to the peritoneum. As vitamin D disrupts the TGF-β/Smad pathway, it may prevent cancer.
Dr. Kitami explains: "The administration of Vitamin D helps normalize the peritoneal environment. This suggests that the combination of Vitamin D and conventional remedies can enhance their therapeutic efficacy for ovarian cancer. We think this helps prevent the adhesion of cancer cells to the peritoneum, which may make it possible to prevent the recurrence of ovarian cancer.”
The potential of a vitamin to combat a cancer that affects one in 75 women remains an exciting prospect, especially since it does so by restoring the natural defenses of the body. The creation of therapies using this research could offer new ways to combat the high death rate of ovarian cancer.
The study, “Peritoneal restoration by repurposing vitamin D inhibits ovarian cancer dissemination via blockade of the TGF-β1/thrombospondin-1 axis,” was published in the journal Matrix Biology on April 26, 2022, at DOI:10.1016/j.matbio.2022.03.003.
Authors:
Kazuhisa Kitami1, *Masato Yoshihara1, Satoshi Tamauchi1, Mai Sugiyama2, Yoshihiro Koya2, Yoshihiko Yamakita2, Hiroki Fujimoto1,3, Shohei Iyoshi1,4, Kaname Uno1,5, Kazumasa Mogi1, Yoshiki Ikeda1, Akira Yokoi1,6, Nobuhisa Yoshikawa1, Kimihiro Nishino1, Kaoru Niimi1, Akihiro Nawa2, Atsushi Enomoto7, Hiroaki Kajiyama1
1 Department of Obstetrics and Gynecology, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan
2 Bell Research Center, Department of Obstetrics and Gynecology Collaborative Research, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan
3 Discipline of Obstetrics and Gynaecology, Adelaide Medical School, Robinson Research Institute, University of Adelaide, Adelaide, South Australia, Australia
4 Spemann Graduate School of Biology and Medicine, University of Freiburg, Albertstr, Freiburg, Germany
5 Division of Clinical Genetics, Lund University, Sölvegatan, Lund, Sweden
6 Institute for Advanced Research, Nagoya University, Nagoya, Aichi, Japan
7 Department of Pathology, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan
Funding:
This study was supported by the Japan Society for the Promotion of Science (JSPS) Grant-in-Aid for Scientific Research (19H03797, 20K03824, 21K16788).
Media Contact:
Matthew Coslett
International Communications Office, Nagoya University
Email: kouho-en@adm.nagoya-u.ac.jp