Medicine, Dentistry, and Pharmacy
October 5, 2022
Researchers develop a new surgical training model for fluorescence-guided cancer surgery using the Japanese food konjac jelly
A research group from Nagoya University has successfully developed a surgical training model using konjac, a processed jelly made from the bulb of the konjac plant. Konjac is commonly used as an ingredient in Japanese cuisine such as shirataki noodles and oden. The group’s training model is a type of tissue-mimicking phantom, which physicians can use to practice fluorescence-guided surgery, an important technique in cancer treatment.
A tissue-mimicking phantom is a surgical training model that mimics human tissue and helps surgeons learn how to perform common surgeries. Developing such a model for near-infrared (NIR) fluorescence is significant because it is potentially an important technique in cancer surgery. In NIR fluorescence-guided surgery, tumor-targeting imaging agents are used to light up parts of the body with fluorescence to guide the surgeon, thereby helping them to see tumors in deep areas.
Other tissue-mimicking phantoms for NIR fluorescence imaging have already been developed. However, these objects were made mostly from gelatin or agarose, which are clinically different from human tissue. As a result, these models are not suitable for training using electrocautery, which requires a heated tool that may damage the training model or create toxic fumes.
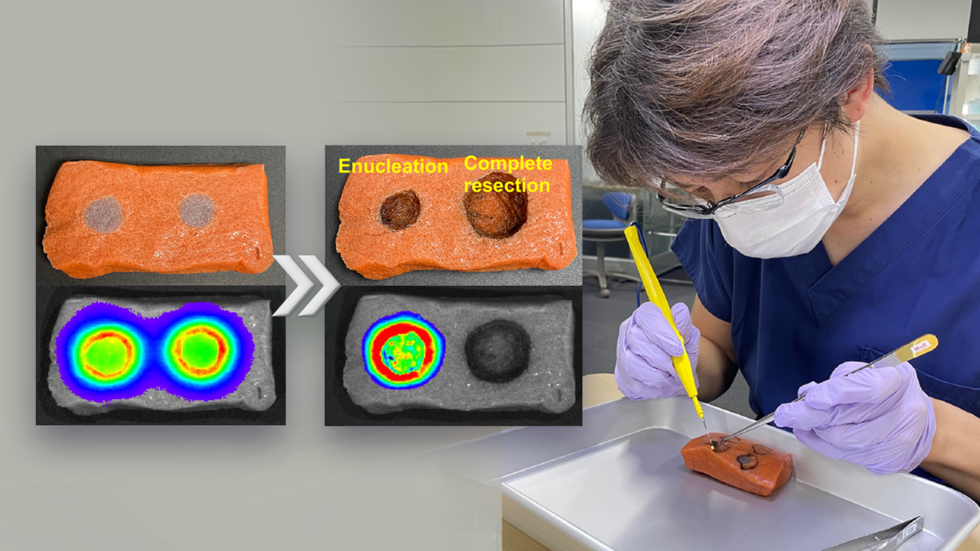
To get around this problem, a group led by Dr. Naoki Nishio, Lecturer at the Nagoya University Graduate School of Medicine, in collaboration with Ehime University in Japan and Vanderbilt University in the United States, has developed a surgical training model for NIR fluorescence imaging using konjac and indocyanine green for fluorescence. To make the tissue-mimicking phantom, the researchers dissolved konjac powder, salt, and paint in water. Next, they added calcium hydroxide to create a paste that was then poured into a dimpled mold to create shapes that resemble tumors and surrounding tissue. Using their tissue-mimicking phantom, the surgeons practiced removing an entire visible tumor, a process called resection, and then also practiced removing a tumor with a 5-mm surgical margin. The study found that their training model is suitable for training surgeons in these two important techniques. The team published their findings in Laryngoscope Investigative Otolaryngology.
“We demonstrated the usefulness of the model in surgery using an electrocautery scalpel used in actual surgery”, Dr. Nishio said. “Our model would be beneficial for surgeons to learn NIR fluorescence imaging and to accelerate fluorescence-guided cancer surgery into clinical application, which is expected to lead to less invasive and more reliable surgical resection. Furthermore, this tumor model is expected to be applied not only to physicians, but also to the development of new products, such as endoscopes equipped with near-infrared light cameras, used in the same surgery.”
“Because our model uses an organic material (konjac),” Dr. Nishio continued, “it is very easy to dispose of after use, making it useful for surgical training for young surgeons and students. The model has many advantages for use during surgical training in fluorescence-guided surgery, including its safety, low cost, easy transportation, and fluorescence stability.”
The surgical training model made of konjac, before (left) and after (right) the tumor resection.
The tumor is visualized under near-infrared fluorescence imaging (bottom).
Image credit: Dr. Naoki Nishio
The study, "Validation of a surgical training model containing indocyanine green for near-infrared fluorescence imaging," has been published in the journal Laryngoscope Investigative Otolaryngology at DOI: 10.1002/lio2.858
Authors:
Naoki Nishio, Sohei Mitani, Kayo Sakamoto, Gaku Moromoto, Sayaka Yokoi, Mayu Shigeyama, Akihisa Wada, Nobuaki Mukoyama, Eben L. Rosenthal, and Michihiko Sone
Funding information:
Hori Sciences Arts Foundation; Japan Society for the Promotion of Science, Grant/Award Number: JP22K09723
Media Contact:
Matthew Coslett
International Communications Office, Nagoya University
kouho-en@adm.nagoya-u.ac.jp