Medicine, Dentistry, and Pharmacy
March 1, 2023
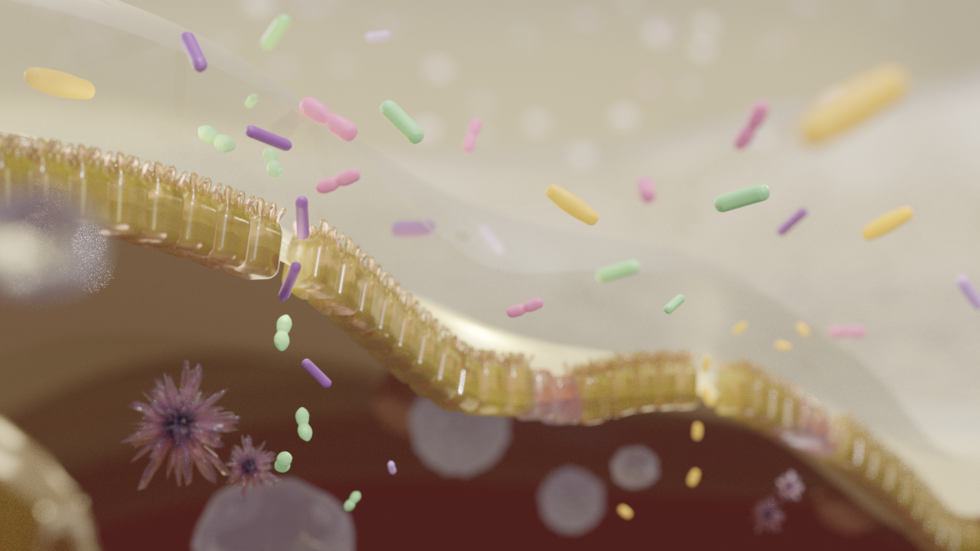
Researchers identify three intestinal bacteria found in dementia with Lewy bodies
Dementia with Lewy bodies (DLB), one of the most common forms of dementia, has no cure. Previous studies suggested that gut bacteria, the microorganisms that live in the human digestive tract, play a role in Parkinson’s disease, another neurodegenerative disorder, but the bacteria involved in DLB had not been identified. Now, a group led by researchers at the Nagoya University Graduate School of Medicine in Japan has identified three bacteria involved in DLB: Collinsella, Ruminococcus, and Bifidobacterium. Their findings, reported in npj Parkinson's Disease, suggest new avenues for diagnosis and treatment.
The onset of DLB is associated with abnormal deposits of alpha-synuclein, a protein in the brain that plays a role in the transmission of signals between neurons. The presence of these deposits, known as ‘Lewy bodies’, affects chemicals in the brain, leading to declines in thinking, reasoning and memory. Symptoms include confusion, memory loss, impaired movement, and visual hallucinations.
Parkinson’s disease also starts with movement problems, but some patients develop cognitive decline within one year. These patients are diagnosed with DLB when this cognitive decline occurs. Physicians find it difficult to predict which people with Parkinson’s disease will develop cognitive decline within a year and become patients with DLB.
A research group led by Associate Professor Masaaki Hirayama (Omics Medicine), Professor Kinji Ohno (Neurogenetics), and Assistant Professor Hiroshi Nishiwaki (Neurogenetics) of Nagoya University Graduate School of Medicine, in collaboration with Okayama Neurology Clinic, Iwate Medical University, and Fukuoka University, analyzed microorganisms in the gut and fecal bile acids of patients with DLB, Parkinson’s disease, and rapid eye movement behavior disorder. They discovered that three intestinal bacteria, Collinsella, Ruminococcus, and Bifidobacterium, were associated with patients with DLB. This may suggest possible ways of diagnosing and treating this neurodegenerative disease.
The researchers also found similarities between the gut bacteria involved in Parkinson's disease and DLB. In both diseases, the bacteria Akkermansia, which degrades the intestinal mucosa, increased. On the other hand, the bacteria that produce short-chain fatty acids (SCFA) in the gut decreased. “Decreases in SCFA-producing bacteria have been repeatedly reported in Parkinson's disease, Alzheimer's disease, and ALS,” explains Ohno. “This suggests that it is a common feature of neurodegenerative diseases.” SCFA are important because they produce regulatory T cells. These types of cells play a critical role in regulating the immune system by suppressing neuroinflammation.
On the other hand, in patients with DLB, the researchers found an increase in Ruminococcus torques, an increase in Collinsella, and a decrease in Bifidobacterium. This was different from Parkinson’s disease patients, whose levels did not change. In the future using these insights, doctors may be able to analyze the bacteria in a person’s digestive tract to distinguish DLB from Parkinson’s disease.
Importantly, the reduced levels of Bifidobacterium may also suggest possible ways to treat DLB. Bifidobacterium increases brain-derived neurotrophic factor, a key protein that supports the growth, development and maintenance of neurons in the central and peripheral nervous systems. Therefore, its decrease in DLB is likely to be associated with cognitive decline.
Similarly, both Ruminococcus torques and Collinsella are intestinal bacteria that carry an enzyme, the product of which regulates inflammation in a region of the brain called the substantia nigra. The substantia nigra produces dopamine, a neurotransmitter that is involved in the regulation of movement and is deficient in Parkinson’s disease. Compared to Parkinson’s disease, the levels of these bacteria were higher in people with DLB. This may explain why the effect on movement is delayed, a key feature that distinguishes DLB from Parkinson’s disease.
“Our findings can be used both for both diagnosis and treatment,” explains Ohno. “If a patient with Parkinson’s disease develops dementia in one year after the onset of motor symptoms, they are diagnosed with DLB. However, we cannot currently predict whether a patient with Parkinson’s disease will become a DLB patient. The gut microbiome will help to identify such patients.”
“In terms of treatment, the administration of Ruminococcus torques and Collinsella in patients with Parkinson’s is expected to delay neuroinflammation in the substantia nigra,” Ohno added. “Therapeutic intervention to increase Bifidobacterium may delay the onset and progression of DLB and reduce cognitive dysfunction.”
“The presence of intestinal bacteria unique to DLB may explain why some patients develop Parkinson’s disease and others develop DLB first,” Ohno said. “Normalizing the abnormal bacteria shared between DLB and Parkinson's disease may delay the development of both diseases. Improving the gut microbiota is a stepping stone in the treatment of dementia. Our findings may pave the way for the discovery of new and completely different therapeutics.”
Researchers have identified gut bacteria that are associated with dementia with Lewy bodies.
Image credit: Reiko Matsushita
The paper, "Gut microbiota in dementia with Lewy bodies," was published in the journal npj Parkinson's Disease on December 9, 2022 at DOI:10.1038/s41531-022-00428-2.
Authors:
Hiroshi Nishiwaki, Jun Ueyama, Kenichi Kashihara, Mikako Ito, Tomonari Hamaguchi, Tetsuya Maeda, Yoshio Tsuboi, Masahisa Katsuno, Masaaki Hirayama, and Kinji Ohno
Media Contact:
Matthew Coslett
International Communications Office, Nagoya University
kouho-en@adm.nagoya-u.ac.jp